Archive for the ‘DEM’ Category
Med-wife crisis
The two legally recognized medical attendants of birth in the US—midwives and physicians—have until recently had starkly different philosophies on the childbearing year. For better or worse, traditional midwives and physicians work in separate worlds. During the trials of labor, doctors operate and midwives cohabitate.
In response to our country’s techno-heavy-attitude towards birth, the space between midwives and physicians has spawned a new role.
It has been sarcastically (and sometimes fittingly) christened the “med-wife”.
Med-wife is a euphemism for a person who has earned the skills and knowledge to practice midwifery, but does so in a gray area that is not quite midwifery and not quite OBGYNery.
For a traditional midwife, birth is safe until proven risky. For a physician, birth is only safe in retrospect. For a med-wife, labor and birth are typically straightforward, but stirrups and episiotomy scissors are always at the ready.
The odds are stacked against the hospital-based midwife. The environment is incompatible with physiological birth, labor care is under the thumb of a large institution, and care-givers are awash in a culture of anticipating problems instead of facilitating healthy birth. Not exactly a recipe for success.
Understandably, it’s difficult to see birth as the natural, normal conclusion to pregnancy when almost every hour of every shift is filled with the kind of drama “A Baby Story” is made of. If narcotic pain management and lithotomy pushing become the norm, traditional midwifery becomes the exception.
Call it Stockholm Syndrome for birth attendants. It makes sense. But it also sets birthing women up to lose.
In the United States, birth might be attended by a Certified Nurse-Midwife (CNM), Certified Professional Midwife (CPM), Direct-Entry Midwife (DEM) or Lay Midwife (LM) depending on the laws of each state and location at time of birth. Of all the qualifications, only a CNM can practice in nearly every state and is welcomed as a primary care-provider in a hospital. All other midwives attend births at home.
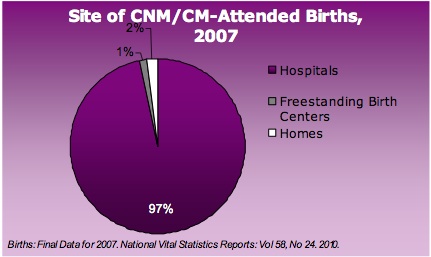
The majority of American women are giving birth in large institutions, and if they choose a midwifery practice, they will be supported by a CNM. This might sound like a wonderful middle-ground, a way to have all of the comforts of a home birth with all the emergency back-up of a hospital birth, but it’s hard to have your cake and eat it too. Or in this case, pie.
The pie chart above, from the American College of Nurse-Midwives (ACNM), illustrates the most recent data ACNM has about birth in the U.S. The fact sheet states that of the 4+ million births that unfolded in the US in 2007, CNMs attended 7.3% of them. Of those births attended by CNMs, 97% took place in hospitals, 2% at home and 1% in free standing birth centers.
With very little exposure to physiological labor and birth, how many of CNMs have the skill set to support a natural birth? How many CNMs resort to commandeering the labor of women instead of navigating labor alongside women—because it’s what institutionalized birth reinforces?
One of the first things the natural birth community teaches the newly enlightened is this: midwives provide the most appropriate prenatal care, labor attendance and postpartum care for the majority of women. When a midwife is a med-wife, when she hovers between medical vigilance and maternalistic guidance, is she inclined to promote healthy birth and provide evidence-based care?
In Denis Walsh’s “Evidence-based Care for Normal Labour and Birth”, she summarizes the growing issue of techo-birth and discusses possible solutions. In her chapter on Birth Setting and Environment, Walsh says that “student midwives and practicing midwives need opportunities to attend home births regularly to address the ‘fish can’t see water’ syndrome of modern maternity services (Wagner, 2001).”
Walsh goes on to explain the theory. “Marsden Wagner’s metaphor refers to blindness generated by constant exposure to one way of doing birth so that it becomes normative in the practitioner’s experience, rendering her unable to envisage or appreciate the alternative.”
She also highlights the response of a segment of the traditional midwifery community. “The Midwives Association of North America (MANA) recognized this pitfall when they developed their pre-registration qualification for midwifery. With their strong roots in apprenticeship-style training, they made it mandatory for students to attend ten out-of-hospital births at home or at birth centers.”
The future of traditional midwifery, as well as the growth or decline of med-wifery, hinges on both the desires of laboring women and the experiences of the care-givers. Just like a healthy economy depends on the mechanism of individual choice, so does birth. The attitude of high-tech-low-touch medical care during labor and birth will become more pervasive if American women continue to (knowingly or unwittingly) choose med-wifes as primary care-givers during the childbearing year.
Getting to know your care-giver well before labor starts is key to ascertaining whether or not she/he is in tune with your wants, needs and desires. Interviewing a medical professional during pre-conception or pregnancy can give you a clearer idea of her/his skills, comfort level and philosophy. Ask a few questions before committing to a care-giver’s practice. It can save you a great deal of frustration and anxiety before, during or after birth—and separate the midwifes from the med-wives.
Some questions to get the dialogue going…
1. Please tell me about your education, experience and philosophy…
What do you think a low-risk pregnancy, labor and birth look like?
What kind of births have you attended [home, birth center, hospital]?
How does/did your college or organization promote and pursue healthy pregnancy and birth for low-risk women?
If a woman expressed a desire for an unmedicated birth [no induction, no drugs], how would you support her prenatally?
- How would you support her and her partner during labor and birth?
2. Please tell me about your prenatal care…
Do you recommend or require prenatal testing or screening?
- If so, which tests? And why? What if I do not want these tests?
If a test came back with a worrisome report, what would be your recommendation for treatment/resolution/management of the condition [Group Beta Strep, Gestation Diabetes]?
Do you recommend pre-labor vaginal exams at the end of pregnancy? Why?
- What if I don’t want any pants-off exams?
What is the average length of pregnancy for your clients, especially first time moms?
Do you recommend your clients attend childbirth education classes?
- Which classes? Why?
If my baby were breech at 36 (or 38 or 41) weeks, what would you suggest?
Do you counsel expectant women or couples on routine male circumcision?
- What do you recommend? Why?
3. Please tell me about the last five births you attended…
Did you know your client very well prior to labor beginning?
- Could you recognize her face and recall her name without her chart?
What kind of fetal monitoring did you recommend [type of equipment used, length of monitoring, frequency of monitor use]?
Did you suggest that any of your clients agree to induction? Why? What kind of induction [AROM, cervical ripener, foley catheter, Pitocin]?
What kind of pain management did your clients ask for [bath/shower, TENs unit, birth ball, rocking chair, positional change, counter pressure, IV narcotics, epidural]?
- What kind of pain management did your clients use/receive?
- Did you suggest alternatives before narcotics were used?
How often do you suggest vaginal exams during labor? Why?
How many births ended…
- Vaginally?
- Surgically?
- With instrumental assistance [vacuum, forceps]?
- With episiotomies?
- With significant tearing?
If it was a vaginal birth, what positions were your clients in during pushing and birth?
- Was this the position your client chose or was she asked to assume this position?
- Did she change positions during pushing? Why or why not?
On average, how long did each mom spend skin-to-skin with her baby immediately after birth? If mom and baby were separated, why?
If it was a surgical birth, were you able to accompany your client into the OR?
- If you were, what kind of support did you offer before, during and after surgery?
- If you were not, why? What kind of support did you offer before and after surgery?
- After surgery, how long did each mom spend skin-to-skin with her baby immediately after birth? If mom and baby were separated, why?
If you work with an OBGYN, why did you choose this person as your consultant?
- How often do you consult with this person during a low-risk labor and low-risk birth? When does consultation become necessary?
4. Please tell me about your postpartum care…
Of your 5 most recent clients, how many are exclusively breastfeeding?
What kind of breastfeeding support/advice do you offer?
Do you have any specialized training to support breastfeeding moms who are experiencing difficulties?
On average, how long does a postpartum client breastfeed her baby [3 weeks, 6 months, 2 years]?
If I were needing support or guidance with self-care, baby care or breastfeeding during non-office hours, what would you recommend I do? Who would you recommend I call?
What kind of birth control do you recommend? What if I wanted to try natural family planning?
How many of your clients return to your practice for subsequent pregnancies?
How many new clients are referred to you by established clients?